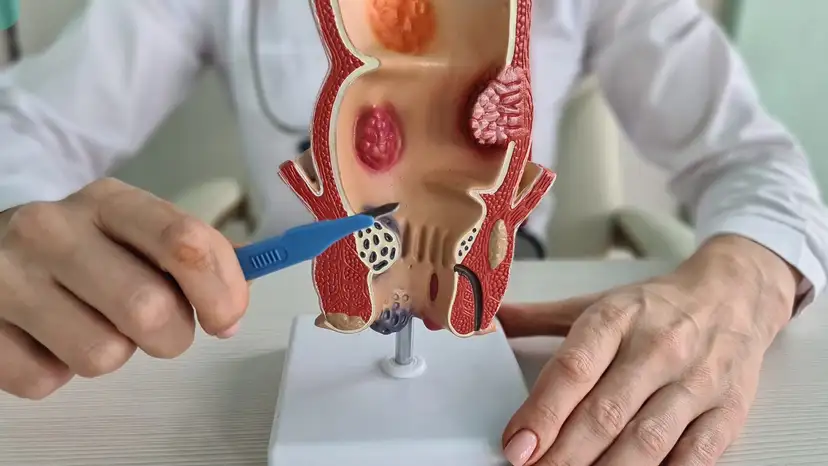
Anal fistulas are abnormal connections that develop between the anal canal and the skin near the anus. They typically form after an infection in the anal glands that fails to heal completely. Patients often experience discomfort, recurrent drainage, and sometimes pain during bowel movements. Anal fistulas can significantly affect daily life if left untreated, leading to persistent irritation and an increased risk of infection. Understanding the condition early allows for timely medical intervention. Various factors contribute to fistula formation, including chronic inflammation, Crohn’s disease, previous abscesses, or trauma to the anal area. Recognizing early symptoms such as swelling, discharge, or persistent pain is crucial for effective treatment.
Surgical repair remains the most effective solution for managing anal fistulas, with multiple approaches tailored to the type and complexity of the fistula. Fistulotomy involves cutting open the fistula tract to allow it to heal from the inside out. Fistulectomy removes the entire fistula tract, which may be preferred in more complex or recurrent cases. Sphincter-sparing techniques are increasingly popular as they reduce the risk of affecting bowel control while promoting healing. Minimally invasive approaches, such as video-assisted anal fistula treatment or laser therapy, offer faster recovery times with reduced tissue damage. Surgeons decide the best procedure based on factors like fistula location, length, and involvement of the sphincter muscles. Patient-specific considerations, including overall health and previous surgeries, also influence the surgical plan. With proper surgical intervention, patients can achieve significant relief and minimize the chances of recurrence.
Recovery after anal fistula surgery requires careful attention to wound care and lifestyle modifications. The initial weeks often involve discomfort, minor bleeding, and drainage, which are normal parts of the healing process. Pain management is essential, and doctors may recommend medications or topical treatments to ease discomfort. Proper hygiene of the surgical area is crucial to prevent infections and support optimal healing. Patients are usually advised to avoid strenuous activities and heavy lifting during recovery. A diet rich in fiber and adequate hydration helps maintain soft bowel movements, reducing strain on the surgical site. Follow-up appointments are critical for monitoring progress and addressing any complications early.
Preventing repeat infections after anal fistula surgery is a priority for long-term success. Recurrent fistulas often result from inadequate healing, poor hygiene, or underlying health conditions. Patients can significantly reduce their risk of recurrence by adhering to proper anal care routines. Diet and lifestyle play a role in prevention, with high-fiber foods promoting regular bowel movements. Early recognition of symptoms such as swelling, increased drainage, or unusual pain allows for prompt medical attention. Maintaining scheduled follow-ups with a colorectal surgeon ensures that any potential complications are detected and treated early. Additionally, patients should avoid self-treatment or unverified remedies that may worsen the condition.
Strategies for preventing repeat infections include:
- Cleaning the anal area gently with warm water after bowel movements
- Avoiding harsh soaps or wipes that can irritate the skin
- Maintaining a high-fiber diet to prevent constipation
- Drinking plenty of water to keep stools soft
- Wearing loose-fitting clothing to reduce friction
- Monitoring for early signs of infection and seeking prompt medical care
- Following all postoperative care instructions provided by the surgeon
Complications after anal fistula surgery, while uncommon, can include delayed healing, persistent drainage, or infection. Recognizing warning signs early can prevent more serious issues. Patients should report excessive bleeding, fever, or severe pain to their healthcare provider immediately. Risk management during recovery involves adhering to wound care protocols, avoiding heavy lifting, and maintaining proper nutrition. Surgeons may provide tailored instructions for activity restrictions based on the type of procedure performed. Effective communication between patient and surgeon is critical to ensure smooth healing. By staying proactive, patients can reduce the likelihood of complications and support successful outcomes.
Supporting overall anal health goes beyond surgery and recovery. Strengthening pelvic floor muscles may aid in maintaining continence and supporting tissue health. Consistent hydration and a balanced diet help promote regular bowel movements, reducing strain on sensitive areas. Individuals with chronic conditions like Crohn’s disease should work closely with their healthcare team to manage inflammation and prevent recurrence. Maintaining good personal hygiene and monitoring for early symptoms are simple yet effective preventive measures. Patients should also consider lifestyle modifications such as limiting prolonged sitting or excessive straining. These steps contribute to long-term anal health and reduce the chances of new fistulas forming.
Adapting daily routines to accommodate healing is an important aspect of recovery. Patients often need to modify physical activity, seating habits, and bathroom routines temporarily. Pain management techniques, including sitz baths or prescribed medications, can improve comfort during the healing process. Emotional and psychological support is also valuable, as dealing with an anal fistula can be stressful. Engaging in gentle exercise, maintaining social connections, and seeking guidance from healthcare professionals can improve overall wellbeing. Clear communication with caregivers or family members ensures adherence to care instructions. Over time, these adjustments help patients regain normalcy while protecting against future infections.
Frequently Asked Questions (FAQ)
- How long does it take to fully recover from anal fistula surgery?
Recovery typically ranges from 4 to 12 weeks, depending on the complexity of the fistula and the surgical method used. Minor discomfort and drainage may continue during the early stages of healing. - Can anal fistulas heal without surgery?
While some small fistulas may heal spontaneously, most require surgical intervention to prevent chronic infection and recurrence. Non-surgical options alone are usually insufficient for long-term resolution. - What are the chances of a fistula coming back after surgery?
Recurrence rates vary based on the type of surgery and fistula complexity. Following postoperative care instructions and maintaining anal hygiene significantly reduce the likelihood of recurrence. - How can I prevent infections during the healing process?
Gentle cleaning, sitz baths, a high-fiber diet, proper hydration, and avoiding straining during bowel movements are effective preventive measures. - Are there non-surgical alternatives to repair anal fistulas?
Minimally invasive treatments like laser therapy, fistula plugs, or VAAFT may be options for select patients, but surgery remains the most reliable method for complete repair. - Will surgery affect bowel control or continence?
Most modern surgical techniques aim to preserve sphincter function. The risk of incontinence is low, particularly with sphincter-sparing procedures. - What lifestyle changes can reduce the risk of recurrence?
A diet high in fiber, proper hydration, regular bowel habits, good hygiene, and prompt management of any infections help prevent recurrence.
Takeaway
Anal fistula surgery is a highly effective approach for resolving persistent fistulas and preventing recurrent infections. Understanding the types of surgical procedures, proper recovery practices, and strategies to maintain anal health are key to long-term success. Patients who follow recommended care routines, monitor for early warning signs, and make lifestyle adjustments experience fewer complications and reduced recurrence. With a proactive approach, it is possible to regain comfort, restore daily activities, and minimize the risk of repeat infections, supporting overall wellbeing and quality of life.